The use of Androgen Therapy in women’s health is a hotly debated topic. Here’s what we know today.
Androgens are typically recognized as male hormones, but in fact testosterone and its biochemical precursor dehydroepiandrosterone (DHEA) are also very important in women’s health.
Androgens have been studied in various gynecological and sexual disorders since the late 1930s. While early investigation of testosterone and DHEA use in women was reported for abnormal menses bleeding, menses cramping, menopausal symptoms, and mood disorders, modern day use of androgens in women has primarily focused on sexual dysfunction treatment for women after the age of menopause or for women who have had their ovaries removed at any age.
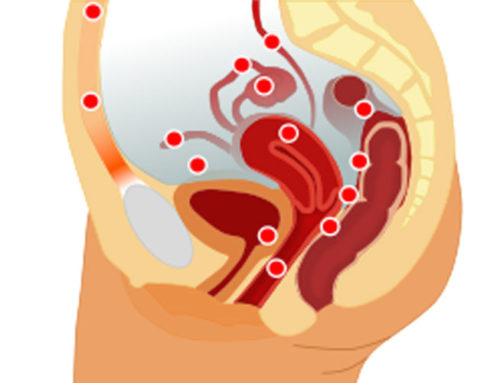
Women produce DHEA and testosterone in addition to estrogens and progesterone. Androgens in women are produced by the ovaries and adrenal glands on a continual basis. DHEA is converted into testosterone in peripheral body tissues, and both DHEA and testosterone can convert into estrogens. Women produce 5-10 percent the quantity of androgen than that of men. Women who have their ovaries removed (oopohorectomy) can result in an immediate 50 percent reduction in circulating serum testosterone, and DHEA.
Female sexual dysfunction is a multifactorial condition that requires careful evaluation and may involve several management strategies, yet the hormonal profile of a woman after menopause with sexual concerns is part of the assessment to determine the origins of sexual dysfunction. Testosterone and DHEA can be one cog of a big wheel related to female sexuality as we age. Androgen therapy in aging women is primarily aimed to enhance interest in initiating sexual activity and response to sexual stimulation.
Androgen therapy however is not FDA approved in the United States, and therefore all testosterone and DHEA therapies prescribed to women are done so off label and are not covered by medical insurance. DHEA can be found over the counter, while testosterone therapy is a controlled substance in the United States and requires a prescription by a physician authorized to prescribe controlled substances. Because testosterone is not FDA approved for use in women, all testosterone products used in women are off label. The primary prescription recommended by medical guidelines is a testosterone gel product that is made for use in men, but is prescribed in female appropriate doses. Testosterone can also be given as an intramuscular injection and hormone pellets inserted into fatty tissue of the buttock.
Yet the use of androgen therapy in women has long been controversial. While safety data for testosterone and DHEA therapy in women has been reassuring to date, and does not appear to increase the risk of breast cancer or cardiovascular disease, longitudinal studies remain needed. The most common side effects of androgen replacement in women are acne or greasy hair.
Efficacy data on how effective testosterone and DHEA therapy is in improving sexual function in women is mixed. Surgically induced as well as naturally menopausal women treated with androgen therapy have the greatest amount of medical literature to support efficacy in reclaiming sexual function. These women have been shown in numerous studies to experience significant increase in satisfying sexual activity decreases in personal distress, and enhancement in overall well-being. Women of reproductive age have the least amount of science suggesting that treating with androgen therapy will be beneficial.
In 2014 a Task Force appointed by the Endocrine Society, American Congress of Obestricians and Gynecologists (ACOG), American Society for Reproductive Medicine (ASRM), European Society of Endocrinology (ESE), and International Menopause Society (IMS) produced a medical practice guideline for the therapeutic use of androgens in women. After extensive review of medical literature, they recommended against making a diagnosis of androgen deficiency syndrome in healthy women because of a lack of a well-defined syndrome, and stated that data correlating androgen levels with specific signs or symptoms is inconclusive.
This same guideline did suggest that evidence supports the short-term efficacy and safety using androgen therapy to replace values to physiological ideal levels in postmenopausal women with low libido. But they did note that serum androgen levels did not predict response to therapy, and furthermore excessively high levels of testosterone and DHEA have not been found to be beneficial. They recommended lastly that all women undergoing off label androgen therapy should be closely monitored by a physician with experience prescribing androgen for women.
In 2019, the first Global Consensus Guidelines on the use of testosterone therapy in women were published (https://www.medscape.com/viewarticle/917561). Multiple international medical societies convened to conclude decades of research summarize that existing evidence clearly shows that testosterone is beneficial in the treatment of sexual desire dysfunction in women after menopause, but not for any other conditions or symptoms, the authors conclude. Findings were similar to the earlier 2014 guidelines, and confirmed safety data to date is reassuring but lacking long term research, blood tests alone do not correlate directly to symptoms but should be used to monitor treatment, and reiterated that clinical applications of effective testosterone replacement therapy is indicated for women after the age of menopause.
Androgen Therapy for women
So how much of “her” should be in androgen therapy? After managing androgen replacement for hundreds of women, my experience has taught me testosterone and DHEA can be novel treatments for some women as they age, but certainly not for all.
Sexual function, energy levels, and mood complaints are often composed of complex medical as well as psychosocial contributions, and hormone evaluation should certainly be part of the consideration when women are seeking to improve their overall well-being. Reproductive age women typically have more than adequate testosterone and DHEA levels, however some forms of hormonal birth control can increase binding globulins which consequently decreases the availability of testosterone levels, resulting in decreased androgen type symptoms.
Many medications such as antidepressants can have sexual side effects and cause symptoms similar to low androgen levels. How much fun or play we have in our lives and in our intimate relationship can have enormous impact on how interested we are in sex, and the health and closeness of our relationships has never-ending impact on our sexual satisfaction.
A woman’s sexual health is always composed of a milieu of factors, one of which can be testosterone and DHEA levels. Furthermore every woman responds differently to hormone therapy, and her personal medical history as well as family history needs to be taken into account as to how effective and safe testosterone or DHEA therapy may be for her. The quality of a testosterone and DHEA product and route of administration can change the symptomatic outcome significantly. Any women undergoing testosterone replacement should have consistent medical monitoring.
Testosterone has been clearly shown to cause fetal harm, this is yet another important factor to discourage inappropriate use of testosterone in younger women. Ultimately androgen therapy has been prescribed by health-care professionals engaged in the management of women’s health issues throughout much of the 20th century. Despite this clinical use of testosterone and DHEA in women for more than seven decades, contemporary androgen therapy in women is hotly debated, often misunderstood, and can be misrepresented in the medical community. Whereas androgen levels should not be considered the only factor involved in midlife women with sexual concerns, it certainly is one important contribution for consideration.